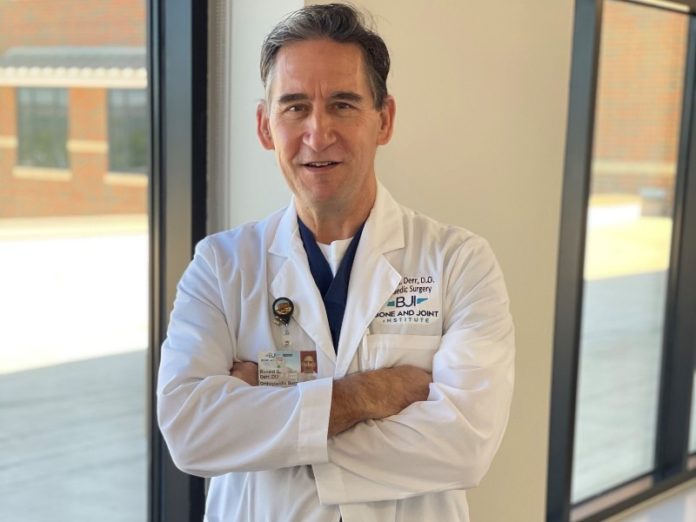
Stress fractures are some of the most common sports and orthopaedic injuries. We recently sat down with Dr. Ron Derr at Bone and Joint Institute of Tennessee to discuss these lower extremity injuries and learn about the treatment options available to patients.
WS: What is a stress fracture? How are they caused?
Dr. Derr:
A stress fracture is an overuse injury where the injury to the bone is occurring at a faster rate than the repair process. With a little bit of time, the bone gradually starts to weaken. It’s like a paper clip being bent back and forth: there’s not one motion that breaks it, but there’s a weak spot that breaks.
Stress fractures are typically seen in weight bearing bones in the lower extremities. Most people who develop them are running, jumping, or doing other athletic activities. Sometimes stress fractures can be caused just by walking or starting an exercise program at a faster clip than your body has had time to adjust to. My advice to patients is that you have to acclimate to activities. Instead of going out and running a bunch of miles, start with walking and shorter distances. Cross train, gradually ramp up activities. Avoid going from zero to 60 so quickly that you get yourself injured.
Poor shoe wear can be a factor. Old shoes that don’t provide good cushion or support can lead to overload of a weight bearing bone, resulting in a stress fracture.
WS: What symptoms might prompt someone to see an orthopaedist?
Dr. Derr:
The first symptom is usually pain. Sometimes both pain and swelling. Most of the time patients have a pain episode that limits their activity and they can’t be fully functional because they’re being held back by their discomfort. Usually point pressure in one area of the ankle, foot, or leg is observed during evaluation, indicating where the injury occurred.
It’s as much a clinical diagnosis as anything. When we x-ray someone with a suspected stress fracture, the bone injury might not show up for 2-12 weeks, sometimes not at all. So just the suspicion of a stress fracture, accompanied by pain and symptoms, might be how we diagnose it. The next best way we can diagnose a stress fracture that doesn’t show up with x-ray is with MRI. A positive MRI finding, however, may not change the treatment plan.
WS: What treatments are available?
Dr. Derr:
The first thing is to stop the activity that’s leading to the stress fracture. The patient must back off from running, jumping, and weight-bearing activities. Stop doing the activity leading to the injury. Non-weight bearing activities, such as swimming, rowing, and stationary bike-riding are great ways to let your injury recover. We’ll often put patients in a walking boot to help spread out the force and minimize the pressure. Ice and elevation will help, as will anti-inflammatories, if directed by your doctor.
WS: What else can be done for stress fractures?
Dr. Derr:
The biggest thing I’ve started doing in the last 10 years is being very aware and sensitive to the patient’s vitamin D level. We’ve found there’s a lot more vitamin D deficiency in the public than you would think. One reason is that sunscreen use minimizes vitamin D uptake and most people are probably not consuming adequate amounts of foods fortified with vitamin D. Children often play inside on a computer rather than playing outside with friends. One reason vitamin D is so important is that it’s necessary for absorbing calcium, which is critical for bone health.
If we have a stress fracture that’s not healing in a timely manner, we’ll use a bone stimulator, a device that helps to increase metabolism of the bone. You don’t see, hear, or feel anything, but it creates a physiologic stimulus that the bone cells respond to. The stimulator is a device that is used at home; it may be used for 20 minutes to three hours a day, usually for several months. Use of this device is not very common for stress fractures in the foot.
If we find that the patient’s weight-bearing mechanics are not the best – flat-footed or a high arch, for example – getting a custom-made orthotic that helps to balance out stresses and spreads the force throughout the foot is another really good option.
WS: How often is surgery necessary for treating stress fractures?
Dr. Derr:
Very rarely. The only time we do surgery for a stress fracture is if the bone is not healing or if the stress fracture allows the bone to angulate, changing the weight-bearing mechanics of the foot in a way that we think would be conducive to further issues later down the road. Surgery is usually not a first line treatment for stress fractures.
WS: What role does physical therapy play in recovery?
Dr. Derr:
It’s an important part. Sometimes there can be muscle imbalance, tightness or weakness that creates a mechanical situation where the stress fracture is more likely to occur. We use physical therapy to mitigate muscle weakness and tightness, working on gait and balance.
WS: What do you enjoy most about your work?
Dr. Derr:
I think the most rewarding thing is to talk with a patient, know they’re struggling, and help them find a way to get back to their desired quality of life. If that occurs, it is very rewarding. Our goal is always to help patients be as mobile and functional as possible with as few limitations as possible. A lot of the time it’s just educating the patient on what needs to be corrected. Most people are good at following those directions and getting back to a healthy state.
Stress Fracture Care at Bone and Joint Institute of Tennessee
For more information about stress fracture treatment at Bone and Joint Institute of Tennessee, contact Ronald Derr, D.O. Call (615) 791-2630. You can also schedule an appointment online.
Have a question for the Bone and Joint Institute, fill out the form below: